Parents rarely walk into a pediatric dental clinic expecting to discuss the underside of a baby’s tongue. Yet tongue tie and its close cousin, lip tie, are common reasons families land in my chair. Some come because a lactation consultant noticed a tight frenulum during a difficult feeding week. Others arrive after months of reflux, slow weight gain, or a toddler who refuses textures. Occasionally, a school-age child struggles with certain sounds, or a teen can’t keep a lower retainer in place because the tissue pulls too hard. Tongue tie threads through all ages, and a thoughtful evaluation by a pediatric dentist can clarify what matters and what does not.
This topic sits at the intersection of feeding, speech, dental development, and family well-being. Good care demands more than a quick look and a quick snip. It asks for clinical judgment, a calm hand, and supportive follow‑up.
What we mean by tongue tie
Tongue tie, or ankyloglossia, refers to a lingual frenulum that restricts normal tongue movement. The frenulum is a band of tissue that runs from the floor of the mouth to the underside of the tongue. Everyone has one. In some children, it inserts close to the tip of the tongue or is thicker or shorter than average, limiting elevation, protrusion, and lateral movement.
Not every tight frenulum needs treatment. We care when function suffers. For infants, that usually means feeding difficulties. For older children, it can show up as trouble clearing food, adapting to orthodontic appliances, or maintaining oral hygiene. Speech concerns are more nuanced. Many children articulate normally despite a restrictive frenum, while others compensate until demands increase.
Lip tie is similar in concept, typically involving a maxillary frenulum between the upper lip and the gum. Again, function drives decision-making: poor flange during breastfeeding, persistent gap between upper front teeth in later childhood, or difficulty cleaning around braces.
How a pediatric dentist evaluates a possible tie
A comprehensive evaluation starts well before the mouth exam. History sets the stage. I ask about pregnancy and birth, feeding from day one, weight trends, nipple pain for breastfeeding parents, bottle refusal, reflux, noisy breathing, sleep, and body tension or arching. For toddlers and older kids, I ask about gagging, food aversions, pocketing food, choking episodes, snoring, speech therapy history, orthodontic consults, and oral habits like thumb sucking or pacifier use.
The physical exam looks beyond the frenulum. I observe posture, airway signs, nasal breathing versus mouth breathing, and jaw development. Inside the mouth, I assess tongue shape, lift, lateralization, and protrusion; lip flange; palate width and height; dental crowding; soft tissue tone; and how the cheeks and floor of the mouth behave under stretch. I gently elevate the tongue with two fingers or a grooved director, not just ask the child to stick out the tongue. Babies cannot follow commands, so functional testing often happens at the breast or bottle, or with a gloved finger to gauge suction and tongue cupping.
Photographs and short video clips can help track changes over time and support communication with lactation consultants and speech‑language pathologists. In complex cases, I use validated function scales, but I never let a number overrule the lived experience of the family. A score is supportive data, not the whole story.
Signs that deserve attention
Babies tell us a lot if we listen. Frequent clicking sounds during feeding, slipping off the breast, dribbling milk down the chin, prolonged feeds that still end with frustration, poor weight gain, maternal nipple trauma and pain, and unusually gassy or colicky behavior can point to restricted tongue movement. A baby who cannot effectively compress and transfer milk often compensates with jaw tension and suction, which is exhausting for both infant and parent.
In toddlers, ties can show as picky eating with preference for soft foods, gagging on mixed textures, persistent drooling, open‑mouth posture, and a habit of pushing food forward rather than moving it side to side. Oral hygiene becomes a battle if the tongue cannot sweep the cheeks and teeth clean.
School-age children may struggle with certain sounds that require elevation and tip precision, such as t, d, l, n, r, and s, though speech is multifactorial. They may also develop lower incisor recession or a diastema if the frenulum exerts pull on the gum or upper lip. Orthodontists often spot restrictive frena when aligners or retainers lift or when expansion struggles against soft tissue tension.
Families sometimes ask about sleep apnea and tongue tie. Restrictive oral tissues do not cause obstructive sleep apnea on their own, but they can contribute to poor oral posture, low tongue resting position, and mouth breathing. These issues fit into a broader airway picture that includes nasal patency, tonsil size, palate shape, and skeletal growth.
What a pediatric dentist brings to the team
The best outcomes come from collaborative care. Lactation professionals, pediatricians, speech‑language pathologists, bodyworkers, and feeding therapists all see different pieces of the puzzle. A board certified pediatric dentist adds oral development expertise and procedural skill, especially with pediatric laser dentistry. We evaluate dental and skeletal growth, the health of the gums and teeth, and the long‑term implications of a tight frenulum for hygiene, caries risk, and orthodontics. We can also spot red flags that mimic ties, such as low tongue tone, torticollis, cranial asymmetry, or sensory aversions that require therapy rather than surgery.
Families often appreciate that a kids dentistry specialist works in a child‑centered setting. A child friendly dentist adjusts pacing, explains instruments in simple language, and uses behavior guidance techniques that lower anxiety. For infants and toddlers, the environment matters as much as technique. Dim lights, warm swaddles, and a quiet room calm everyone.
When treatment makes sense, and when it doesn’t
I walk families through three paths: watchful waiting with supportive therapy, therapy first then re‑evaluate, or release of the frenum with targeted aftercare. The right path depends on severity and age.
Mild restriction with minimal symptoms often improves as babies grow, especially with skilled lactation support. I have seen newborns labeled “tongue‑tied” in the hospital latch beautifully after two weeks of coaching and positional changes. Conversely, a baby with poor weight gain and severe maternal pain should not wait for months. Function sets the timeline.
Toddlers and older kids with feeding issues often benefit from a short course of feeding therapy or oral motor work to address patterns that have settled in. If progress plateaus because tissue restriction limits movement, a release can unlock further gains.
https://www.instagram.com/949pediatricdentistry.ortho/For speech, I rely on the speech‑language pathologist. If a child can produce sounds with cueing in the clinic but not in daily life, therapy alone may be enough. If the tongue cannot achieve necessary elevation even with therapy, we consider release. We aim to avoid a situation where a quick procedure leaves the child without the motor patterns needed to use the new range of motion. Skill first, then access, then integrate.
How a frenectomy is performed
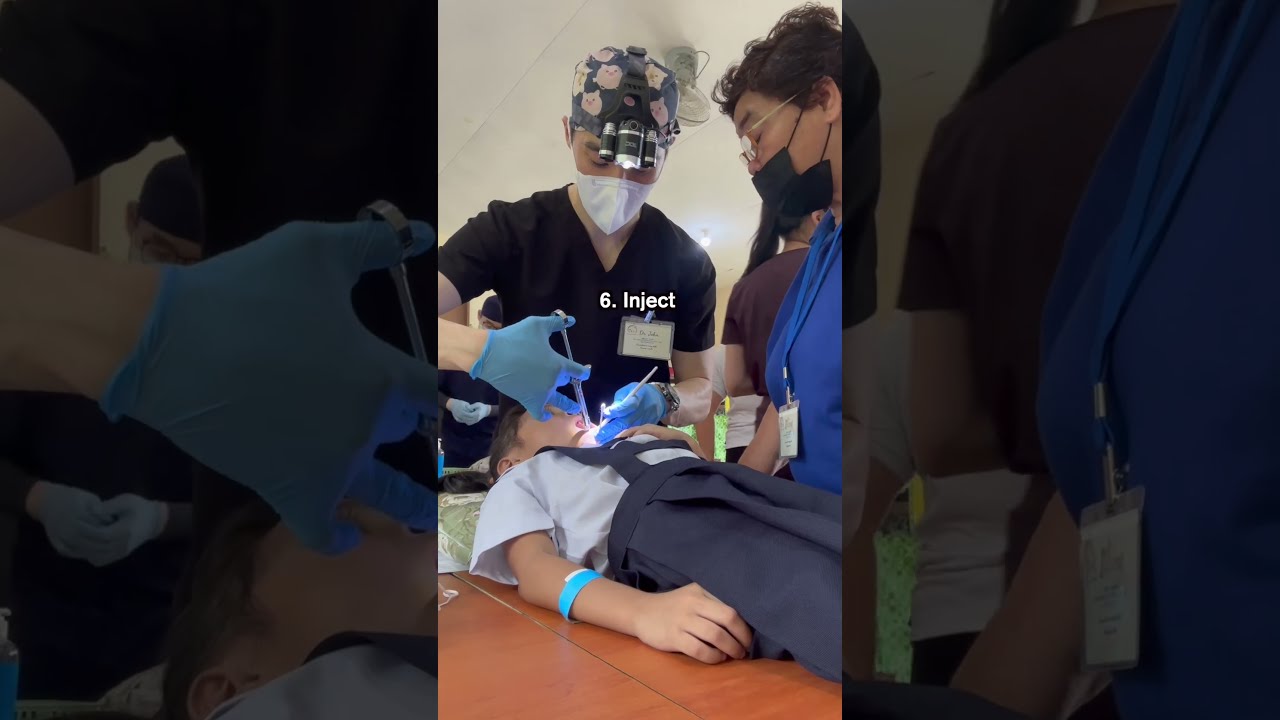
In a pediatric dental office, a frenectomy can be done with sterile scissors or with a diode or CO2 laser. Both work. I choose based on the child’s age, tissue thickness, and bleeding risk. Scissors provide tactile feedback and immediate release, while lasers cauterize as they cut, which can reduce bleeding and operative time. For infants, the entire procedure typically takes a few minutes. For older children, we may spend longer on preparation and teamwork than on the release itself.
Comfort is non‑negotiable. Infants receive a sweet solution and swaddling; some offices offer topical anesthesia for babies, others use a very small amount of local anesthesia depending on the tissue. For toddlers and anxious kids, nitrous oxide can take the edge off. When we treat children with significant sensory needs or with multiple procedures, a sedation pediatric dentist may plan care with oral sedation or, rarely, general anesthesia in a hospital setting. Safety and the child’s well‑being guide this choice.
Bleeding is usually light and stops quickly. Parents often hold and feed immediately in the room. That first latch after release can be emotional. Sometimes it’s dramatically better. Other times, improvement comes over days as soreness fades and the baby relearns a more efficient pattern.
Aftercare that actually works
No two mouths heal the same way. I prepare families for the first 48 hours to be tender. Babies may be sleepier or fussier. Breastfed infants often prefer frequent, short feeds as they adjust. I recommend skin‑to‑skin time, paced bottle feeds if needed, and a lactation follow‑up within 24 to 72 hours.
Stretching or wound care protocols vary by practice and by tissue type. The goal is to minimize the chance of the tissue reattaching tightly while avoiding trauma. I prefer brief, purposeful lifts several times a day, paired with calming strategies, rather than aggressive poking that erodes parental confidence. In older children, gentle tongue elevation and side‑to‑side motion exercises help integrate new range of motion into chewing, swallowing, and speech. The best results happen when families have clear demonstrations, written instructions, and a contact for questions.
Bodywork can be valuable when tension patterns are entrenched. For some babies, a session with a skilled physical therapist, chiropractor, or occupational therapist helps relax the floor of the mouth and neck so the new mobility translates into better function. I suggest targeted therapy, not a long open‑ended plan. We reassess after a few visits.
Risks, limits, and myths
Every procedure carries risk. With frenectomy, the common issues are temporary fussiness, mild bleeding, transient feeding regression, and, less commonly, scarring or reattachment that limits improvement. Infection is rare with proper hygiene. Over‑release can damage adjacent structures, especially near the salivary ducts, which is why experience matters.
Not every breastfeeding problem is a tongue tie, and not every tight frenulum needs to be cut. Oversimplification helps no one. I have met babies who struggled because of oversupply or shallow latch technique, and their feeding normalized without surgery. I have also seen older kids with clear restriction who never learned to elevate the tongue despite years of therapy, and they blossomed after a well‑timed release. The art lies in matching treatment to need.
On speech, a tight tie does not guarantee articulation delay, and release alone does not cure a speech disorder. On orthodontics, a lip tie seldom decides the fate of a midline gap. Timing and growth matter. On airway, a frenectomy is not a cure for snoring or apnea but may be one piece in a comprehensive approach that includes nasal hygiene, allergy care, and skeletal guidance.
Costs, insurance, and practical logistics
Families ask about affordability and coverage at the first call. Policies vary widely. Many dental plans recognize frenectomy codes; some medical plans cover infant releases tied to feeding dysfunction. Practices that are a pediatric dentist that takes insurance or a pediatric dentist that takes Medicaid can verify benefits before the visit so there are no surprises. For those without coverage, pediatric dentist payment plans help spread costs. An affordable pediatric dentist will present options clearly, including splitting therapy and procedure visits when appropriate.
Access matters too. Feeding problems do not wait for a calendar slot next month. Many pediatric dental offices hold space for a same day pediatric dentist visit in urgent feeding cases. A weekend pediatric dentist or pediatric dentist open on Saturday or Sunday can be a lifesaver for latch crises that peak after the workweek. Families searching “pediatric dentist near me” or “baby dentist near me” should ask about availability, experience with infants, and coordination with lactation.
How to choose the right provider
Parents feel overwhelmed wading through online claims and forum posts. Here is a concise way to vet a dentist for kids when tongue or lip ties are suspected:
- Ask how they decide when to treat, and when not to. Look for a function‑first answer and mention of team care. Ask about experience with infants and toddlers, not just older children. Technique and aftercare differ by age. Ask whether they coordinate with lactation consultants, SLPs, and feeding therapists. Good communication improves outcomes. Ask what comfort measures and anesthesia options they use, including nitrous or sedation for anxious kids if needed. Ask for realistic expectations and follow‑up plans. A clear roadmap beats promises of instant fixes.
Online pediatric dentist reviews can be helpful, but weigh them alongside a direct conversation. A kid friendly dentist should make you feel heard, not rushed. The first pediatric dental visit for ties should feel collaborative.
A day in the clinic: what it looks like
A typical morning might include a four‑week‑old who lost weight despite every effort. The lactation consultant joins us. During the evaluation, we see poor tongue elevation, strong compensatory jaw action, and a thick anterior frenulum. After a measured discussion, the parents choose release that day. We use a laser, the baby nurses right away with a deeper latch, and the family schedules follow‑up with lactation for the next afternoon. By day three, the mother reports less pain and audible swallowing.
Later, a two‑year‑old arrives with gagging on solids and speech delays. The exam shows moderate tethering and global oral motor weakness. We choose therapy first. After four weeks of targeted feeding and play‑based oral motor work, progress stalls at lateralization. We perform a gentle release with nitrous in the kids dental clinic, followed by simple exercises and weekly therapy. Over the next month, the child expands to soft meats and mixed textures.
In the afternoon, a 10‑year‑old with orthodontic crowding and a low tongue posture stops by. The orthodontist requested our opinion before starting expansion. The frenulum is tight, but the child has adequate function. We document baseline, start expansion with the children’s dental specialist, and hold off on any release. Six months later, as the palate widens and nasal breathing improves under allergy care, tongue posture improves on its own. No procedure needed.
These vignettes underline the principle that treatment should be tailored, not automatic.
Special considerations for unique kids and family situations
Children with sensory processing differences, autism, or complex medical histories deserve extra planning. A pediatric dentist for special needs children builds flexible schedules, desensitization visits, and visual supports into care. When oral aversion is significant, therapy may precede any oral procedure by weeks. If we proceed, we use the least invasive comfort strategy that keeps the child safe. Sometimes that means a short procedure with nitrous. Sometimes it requires hospital support under anesthesia coordinated with other needed care, like ear tubes or dental treatment for cavities.
Families facing financial stress need respectful options. Practices committed to accessible pediatric dental care can offer scaled fees, payment plans, or assist with claims paperwork. A pediatric dentist accepting new patients who takes time to map out steps reduces the emotional tax on parents who are already stretched thin.
What progress looks like and how to track it
After release, I encourage families to look for trendlines rather than perfection by day one. For infants, the first wins may be less nipple pain, fewer clicks, and shorter, more efficient feeds. Weight gain should reflect effective transfer within one to two weeks. For toddlers, watch for expanding textures, less gagging, and calmer mealtimes over two to four weeks. For school‑age children, look for easier articulation drills in therapy, less drooling, better oral hygiene, and improved tolerance of appliances.
We check in at one week, three to four weeks, and, if needed, two to three months. Photos of the wound bed day by day can prevent anxiety about normal healing color changes. Short videos of latch or chewing patterns are excellent for remote review when a family cannot return promptly.
Beyond ties: the broader value of the pediatric dental home
Even when families visit only for a suspected tie, we use the opportunity to establish a supportive dental home. The first dentist for baby visit typically happens by age one, earlier if concerns arise. Regular preventive care, fluoride varnish when appropriate, x rays only when indicated, and sealants as molars erupt keep cavities at bay. A gentle dentist for kids can also help with space maintainers after early tooth loss, fluoride treatment schedules for high‑risk children, and timely braces referrals.
Life throws curveballs: a chipped tooth at the playground, a tooth injury during sports, a sudden toothache on a Sunday morning. Having a family and pediatric dentist who knows your child makes emergency dental decisions calmer. Practices with an emergency pediatric dentist, 24 hour pediatric dentist triage line, or weekend pediatric dentist hours shorten the time from panic to plan.
Final thoughts from the chair
Tongue tie sits at the edge of several disciplines, which is why opinions can be loud and conflicting. The job of a pediatric dentist is to quiet the noise, examine the child in front of us, and guide families with transparency. If function is fine, reassurance is the best medicine. If function is compromised, we act with skill and restraint, support healing with practical aftercare, and loop in the right professionals at the right time.
If you are searching for a children’s dentist near me or a pediatric dental clinic that understands infant feeding and oral development, ask pointed questions. Look for a calm, evidence‑aware approach that leaves room for your story. That combination, more than any specific instrument or technique, leads to results that matter: babies who feed well, children who eat and speak comfortably, and families who feel seen along the way.
For parents ready to take the next step, schedule a pediatric dentist consultation. Bring your questions, your observations, and, if you have them, notes from your lactation consultant or therapist. A good visit feels like a conversation, not a verdict. And if we decide to move forward, we do it together, at a pace that fits your child.
📍 Location: New York, NY
📞 Phone: +12129976453
🌐 Follow us: